In the realm of cardiovascular health, stents have become a vital tool for keeping arteries open and ensuring proper blood flow to the heart. But a common question that arises among patients and their families is, “How long do stents last?” Understanding the longevity of stents is crucial for anyone who has undergone or is considering stent placement. This article aims to provide a comprehensive guide on the lifespan of stents, factors influencing their durability, types of stents, and how to maintain them for optimal health. By the end of this article, you will have a clear understanding of the durability of stents and the steps you can take to ensure their effectiveness.
What Are Stents?
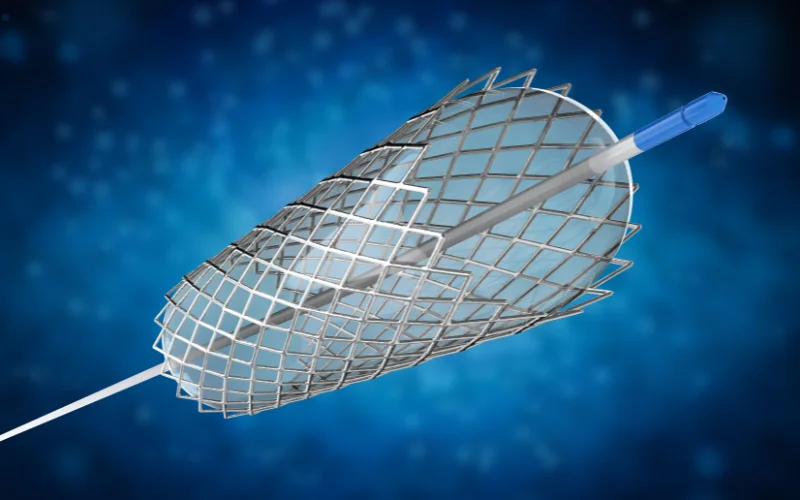
Stents are small, tube-like structures made of metal or plastic that are inserted into arteries or other vessels to keep them open. They are commonly used in procedures like angioplasty to treat conditions such as coronary artery disease.
Stents play a crucial role in cardiovascular procedures, acting as scaffolds to keep arteries open and ensure proper blood flow. They are commonly used to treat conditions such as coronary artery disease. Understanding the different types of stents and their specific functions can help patients make informed decisions about their treatment options.
Function of Stents
The primary function of stents is to act as a scaffold, keeping the artery open and ensuring smooth blood flow. This helps to prevent conditions like heart attacks and strokes by maintaining adequate blood circulation.
Types of Stents
There are several types of stents, each designed for specific medical conditions:
- Bare-Metal Stents (BMS)
- Drug-Eluting Stents (DES)
- Biodegradable Stents
How Long Do Stents Last?
The longevity of stents is a common concern for patients who have undergone stent placement. On average, stents can last anywhere from 5 to 15 years, depending on various factors such as the type of stent, the patient’s overall health, and lifestyle choices. Understanding these factors can help in maintaining the effectiveness of the stent for a longer period.
Factors Influencing Stent Longevity
Several factors can affect the lifespan of a stent:
- Type of Stent: Different stents have different durability.
- Patient’s Health: Overall health and presence of other medical conditions.
- Lifestyle: Smoking, diet, and exercise.
- Medication Adherence: Following prescribed medication regimens.
Stent Location Affect
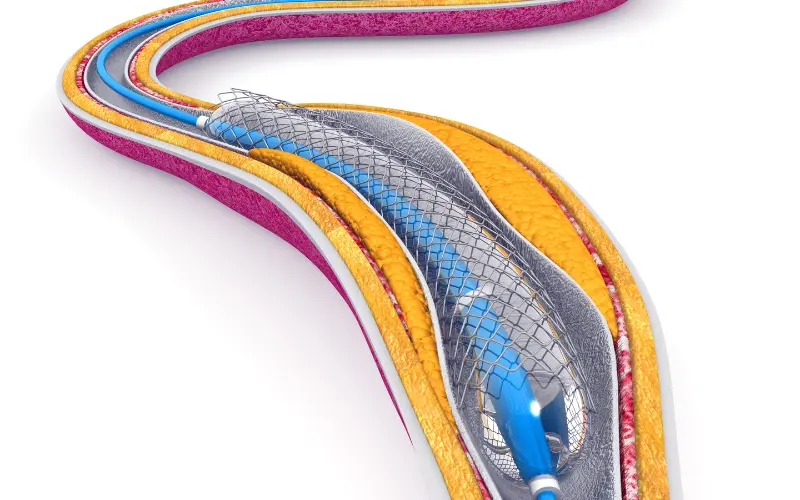
The location of the stent within the body can also influence its longevity. Stents placed in larger arteries may last longer compared to those in smaller, more complex vessels. The environment within the artery, such as blood flow dynamics and pressure, can also impact stent durability.
Types of Stents and Their Longevity

Different types of stents offer varying levels of durability and effectiveness. Bare-metal stents, drug-eluting stents, and biodegradable stents each have unique characteristics that influence their longevity. Understanding these differences can help patients and healthcare providers choose the most suitable stent for each individual case.
Bare-Metal Stents
Bare-Metal Stents (BMS) are the most basic type of stents used in medical procedures. Made entirely of metal, these stents provide a simple scaffold to keep the artery open. While they are effective in preventing immediate artery collapse, they have a higher risk of restenosis, which is the re-narrowing of the artery due to tissue growth over the stent. Typically, bare-metal stents last around 5 to 10 years. They were the first type of stents introduced and are often used in situations where the patient may not be able to tolerate long-term anti-clotting medication.
Drug-Eluting Stents
Drug-Eluting Stents (DES) are a more advanced type of stent that is coated with medication designed to prevent the artery from closing again. The drug coating is gradually released into the artery wall, reducing the risk of restenosis significantly compared to bare-metal stents. Drug-eluting stents can last between 10 to 15 years and have become the preferred choice in many cases due to their effectiveness in maintaining artery openness. However, patients with these stents typically need to adhere to a longer regimen of anti-clotting medications to prevent complications.
Biodegradable Stents
Biodegradable Stents represent a newer innovation in stent technology. Unlike traditional metal stents, biodegradable stents are designed to dissolve over time, leaving no permanent foreign material in the artery. These stents provide temporary support to the artery while it heals and are absorbed by the body within 2 to 3 years. The main advantage of biodegradable stents is that they reduce the long-term risk of complications associated with permanent stents. However, their long-term effectiveness is still being studied, and they are not yet as widely used as bare-metal or drug-eluting stents.
Maintaining Stent Health

Maintaining the health of a stent is crucial for its longevity. This involves making lifestyle changes, attending regular medical check-ups, and adhering to prescribed medications. By taking these steps, patients can significantly improve the lifespan and effectiveness of their stent.
Lifestyle Changes
Adopting a healthy lifestyle is crucial for prolonging the life of your stent:
- Quit Smoking
- Healthy Diet
- Regular Exercise
Regular Check-Ups
Regular medical check-ups are essential for monitoring the condition of your stent and overall heart health. These check-ups typically include imaging tests like angiograms or ultrasounds to ensure that the stent is functioning properly and that there are no signs of complications such as restenosis or stent thrombosis. It is generally recommended to have follow-up appointments every 6 to 12 months, but the frequency may vary based on individual health conditions and the type of stent used.
Medications
Medications play a vital role in maintaining the health of your stent and preventing complications. After stent placement, patients are usually prescribed a combination of antiplatelet medications, such as aspirin and clopidogrel, to prevent blood clots from forming around the stent. These medications help to reduce the risk of stent thrombosis, a serious condition where a blood clot forms at the site of the stent and can lead to a heart attack.
Potential Complications
While stents are generally effective, they can come with potential complications such as restenosis and stent thrombosis. Being aware of these risks and taking preventive measures can help in managing the health of the stent more effectively.
Restenosis
Restenosis refers to the re-narrowing of the artery after stent placement, which occurs when scar tissue forms inside the stent. This can lead to reduced blood flow and the return of symptoms such as chest pain or shortness of breath. Restenosis is more common in bare-metal stents, with an occurrence rate of about 20-30%. Drug-eluting stents have significantly reduced the incidence of restenosis to less than 10% by releasing medication that inhibits tissue growth. Treatment for restenosis may involve additional procedures such as balloon angioplasty or the placement of another stent.
Stent Thrombosis
Stent Thrombosis is a serious and potentially life-threatening complication where a blood clot forms at the site of the stent. This can occur at any time after stent placement, but the risk is highest within the first few months. Stent thrombosis can lead to a sudden blockage of the artery, resulting in a heart attack. Symptoms may include severe chest pain, shortness of breath, and lightheadedness. Immediate medical attention is required if stent thrombosis is suspected. Preventive measures include strict adherence to antiplatelet medications and regular follow-up with your healthcare provider to monitor stent function and overall heart health.
Conclusion
Understanding how long do stents last and the factors that influence their longevity is crucial for anyone who has undergone or is considering stent placement. By following a healthy lifestyle, adhering to medications, and attending regular check-ups, you can significantly extend the life of your stent and maintain optimal heart health. Always consult with your healthcare provider for personalized advice and treatment plans. Taking proactive steps can ensure a healthier, more active life post-stent placement.
FAQs
1. Can a stent be removed once it is placed?
Stents are generally designed to be permanent and are not usually removed. However, in rare cases where complications arise, a stent may need to be surgically removed or replaced.
2. How long does the stent placement procedure take?
The stent placement procedure, also known as angioplasty, typically takes about 1 to 2 hours. However, the exact duration can vary depending on the complexity of the case and the number of stents being placed.
3. Can stents get clogged or blocked over time?
Yes, stents can become clogged or blocked over time due to factors like restenosis (re-narrowing of the artery) or thrombosis (blood clot formation). Regular follow-up appointments and adhering to prescribed medications can help manage these risks.
4. What medications are typically prescribed after stent placement?
Patients are usually prescribed antiplatelet medications such as aspirin and clopidogrel (Plavix) to prevent blood clots. The duration of medication depends on the type of stent and the patient’s individual health condition.